Psoriasis Symptoms: Identifying Rash, Itching, and Skin Plaques
For over 9 years, I’ve sat with people who feel frustrated, misunderstood, and deeply uncomfortable in their own skin.
They show me the red patches on their skin, describe the relentless psoriasis itching that keeps them up at night, and share the emotional toll of having a condition that is so visible, yet so often misinterpreted.
Psoriasis isn’t just “dry skin.” It’s an autoimmune journey, a signal from your body that something deeper is out of balance. My goal today is to walk with you through the landscape of psoriasis symptoms. We’ll demystify what’s happening, help you identify the specific signs, and explore how a holistic, homeopathic approach can offer a path toward lasting relief by addressing the root cause.
What Exactly Is Psoriasis (And Is It Contagious) ?
Before identifying symptoms, it’s crucial to understand what psoriasis truly is. At its core, psoriasis is an autoimmune condition. This means your immune system, designed to protect you, mistakenly goes into overdrive and attacks your own healthy skin cells.
This misguided attack triggers a rapid acceleration of skin cell production. Normally, your skin cells grow and shed over about a month. In a person with psoriasis, this process can happen in just a few days.
Because the body can’t shed these excess cells fast enough, they pile up on the surface. This buildup creates the characteristic psoriasis plaques and scales we see.
A question I hear almost daily is, “Is psoriasis contagious?” Let me be unequivocally clear: No, it is not. You cannot “catch” psoriasis from someone or give it to anyone else. It is an internal, immune-mediated process, not an external infection.
What Does Psoriasis Look Like? Identifying the Early Signs and Symptoms
While psoriasis can vary, most people experience a combination of hallmark symptoms. In my practice, patients often describe a constellation of signs that, together, paint a clear picture.
The most common psoriasis symptoms include:
- Psoriasis Plaques: Raised, well-defined patches of thick red skin. These are the most recognizable sign.
- Silvery Scales on Skin: The plaques are typically covered with white or silvery scales—the buildup of dead skin cells. These can flake off and be particularly noticeable on dark clothing.
- Psoriasis Itching: The itch can range from mild to debilitating. Patients often describe it as a deep, burning, or even biting sensation.
- Burning Sensation: The inflamed plaques can feel hot or like a sunburn.
- Dry, Cracked Skin That Bleeds: The skin within the plaques is extremely dry and can easily fissure or crack, leading to pain and bleeding, especially in areas that bend, like knuckles or knees.
While it can appear anywhere, classic plaque psoriasis is most common on the outside of the psoriasis on elbows and psoriasis on knees. The scalp is another very frequent location.
Beyond the Plaques: Are There Different Types of Psoriasis ?
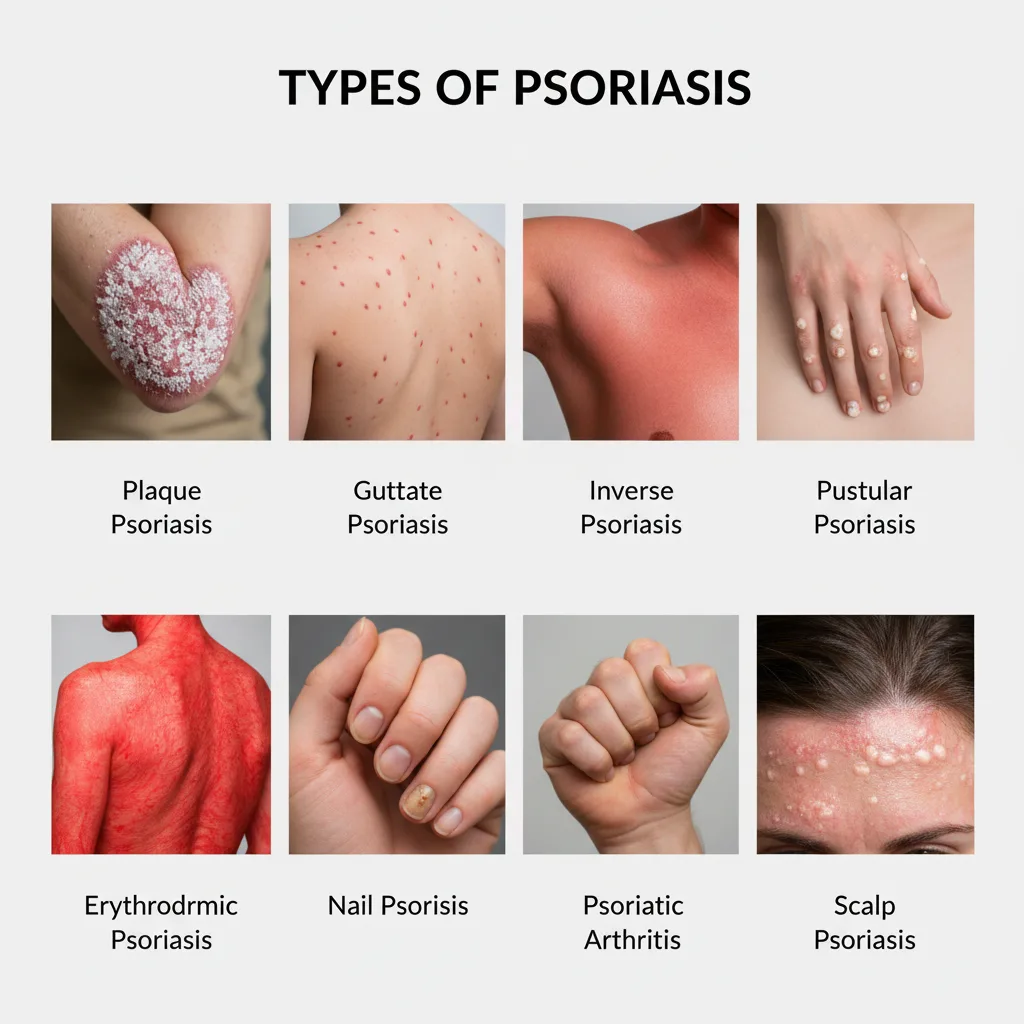
Psoriasis doesn’t look the same on everyone. Recognizing the specific type you have is a key step toward finding the right path to management.
Plaque Psoriasis Symptoms: The Classic Presentation
This is the most common form, affecting 80-90% of people with the condition. It presents as the classic, well-defined plaques with silvery scales we discussed above.
Scalp Psoriasis Symptoms
Often mistaken for severe dandruff, scalp psoriasis causes red patches and silvery-white scaling on the scalp. It can extend beyond the hairline onto the forehead, neck, and behind the ears, causing significant itching and flaking.
Guttate Psoriasis Symptoms
I often see guttate psoriasis appear suddenly, especially in children and young adults after an infection like strep throat. It appears as small, teardrop-shaped, red or pinkish spots on the trunk, arms, and legs.
Inverse Psoriasis
This type affects psoriasis in skin folds—under the arms, in the groin, and under the breasts. Instead of scaly plaques, inverse psoriasis symptoms include smooth, bright-red, and often shiny patches of skin worsened by sweat and friction.
Nail Psoriasis
The nails can be a window into psoriatic disease. Nail psoriasis can cause tiny pits in the nails (nail pitting), discoloration, crumbling, and separation of the nail from the nail bed (onycholysis).
More severe but less common forms include pustular psoriasis and erythrodermic psoriasis, both of which require immediate medical attention.
Can Psoriasis Affect Your Joints? Understanding Psoriatic Arthritis

One of the most critical connections I help patients make is between their skin and their joints. Up to 30% of people with psoriasis will develop psoriatic arthritis (PsA).
This is where the autoimmune attack extends to the joints and the places where tendons and ligaments attach to bone. The biggest challenge is that early signs of psoriatic arthritis can be subtle and easily dismissed as normal aches.
Key psoriatic arthritis symptoms to watch for include:
- Swollen Joints: Pain, swelling, and warmth in one or more joints, often in the fingers, toes, or wrists.
- “Sausage Digits” (Dactylitis): A hallmark sign where an entire finger or toe swells up. This is a very specific indicator of psoriatic arthritis fingers.
- Morning Stiffness: Significant stiffness upon waking that lasts for more than 30 minutes.
- Nail Changes: The presence of psoriatic arthritis nails (pitting, separation) is a strong predictor of developing PsA.
- Lower Back Pain: Inflammatory back pain that improves with activity but worsens with rest.
- Heel and Foot Pain: Pain at the back of the heel (Achilles tendinitis) or on the sole of the foot (plantar fasciitis).
If you have psoriasis and are experiencing any of these joint-related symptoms, it confirms the disease process is systemic, reinforcing the need for a deep, constitutional approach.
How Can You Tell the Difference Between Psoriasis and Eczema?
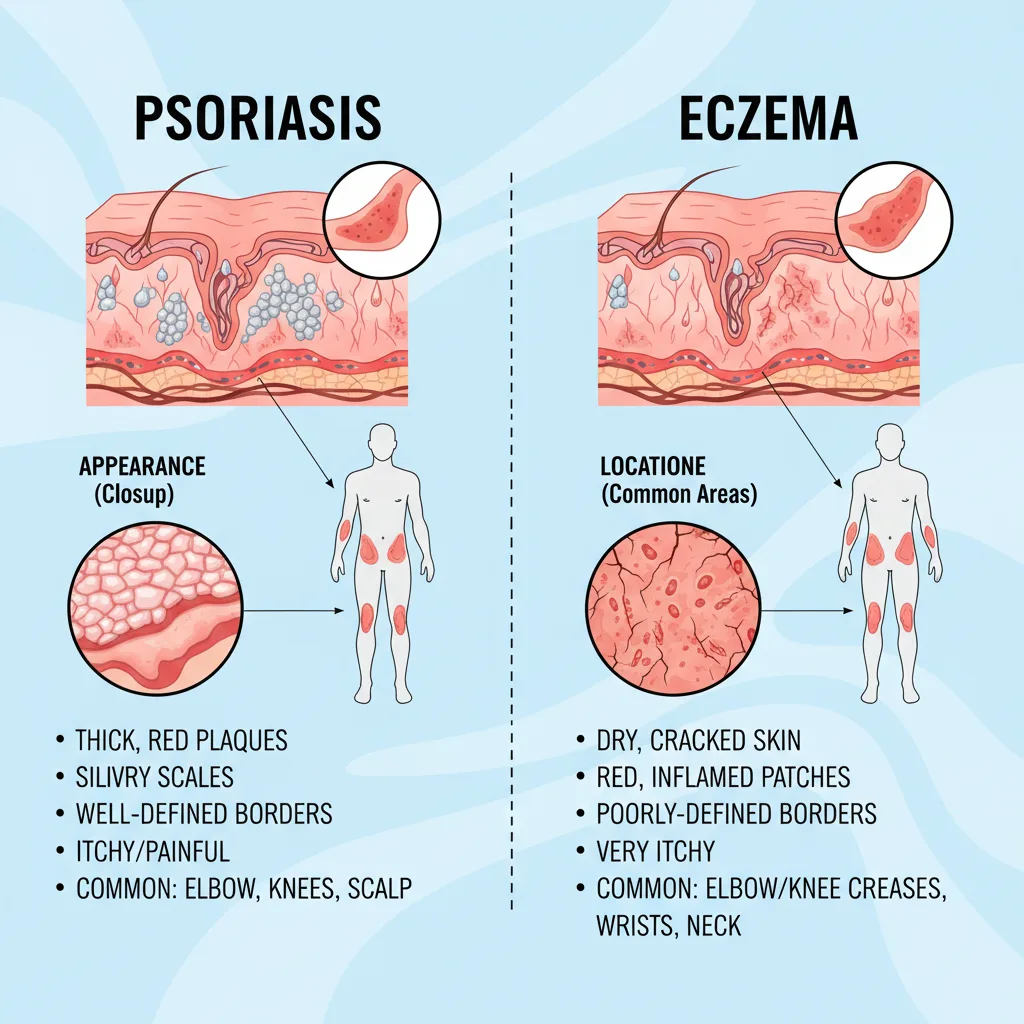
Many patients come to me confused, having been told they might have eczema, psoriasis, or both. While they share some similarities, there are key differences a trained eye can spot.
| Feature | Psoriasis | Eczema (Atopic Dermatitis) |
|---|---|---|
| Itch | Often a burning or stinging sensation. | Typically a very intense, frantic itch. |
| Appearance | Well-defined, raised plaques with thick, silvery scales. | Ill-defined borders. Skin may be weepy or crusted. |
| Location | Commonly on elbows, knees, scalp (extensor surfaces). | Commonly inside elbows, behind knees (flexor surfaces). |
| Skin | The skin is thick and inflamed. | Skin can look thinner from chronic scratching. |
How Does a Homeopathic Approach Address Psoriasis Symptoms?
Conventional treatment often focuses on suppressing symptoms with steroids or drugs that inhibit the immune system. While sometimes necessary, these approaches don’t always address the why.
Homeopathy works differently. My job as a homeopath is to understand your unique expression of psoriasis. I don’t just see “psoriasis”; I see you.
I need to know:
- What makes your itching better or worse?
- Are your symptoms tied to stress or weather?
- How does it affect your sleep and your mood?
Based on this complete picture constitutional homeopathic remedy is chosen. This remedy is designed to gently stimulate your body’s own healing mechanisms, rebalancing the immune system from within rather than just silencing its symptoms. This approach is detailed further in our guide to Homeopathic Treatment for Psoriasis.
The aim is to calm the autoimmune response at its root, leading not just to clearer skin, but to improved overall well-being.
Understanding Your Body’s Signals
Recognizing these psoriasis symptoms in yourself can be overwhelming, but it is also an act of empowerment. It’s the first step on a journey toward taking back control. Your skin is communicating with you, and now you have a better understanding of its language.
If what you’ve read today resonates with your experience, know that you are not alone and that a holistic path to relief exists.
If you would like personalised guidance, speak to a qualified homeopathic practitioner for a full assessment.

